Increase in Candida auris and Carbapenemase-producing Organisms
Dear Colleague,
The Virginia Department of Health continues to respond to reports of cases and outbreaks of Candida auris (C. auris) and/or carbapenemase-producing organisms (CPOs). C. auris is an emerging fungus that presents a serious global health threat. It is often resistant to antifungal drugs used to treat Candida infections and can cause outbreaks in healthcare settings. This advisory provides an update on the current epidemiology of these organisms in Virginia and recommendations for prevention and control.
VDH is observing a concerning increase in C. auris and CPO cases in Virginia. While most reported cases of C. auris and CPOs remain concentrated in Northern Virginia, increasing cases and outbreaks in the Central Region and detection of cases in all regions of Virginia indicate healthcare facilities across the state should be on alert for C. auris and CPOs. Case data and additional information can be found on the VDH C. auris and VDH CPO websites.
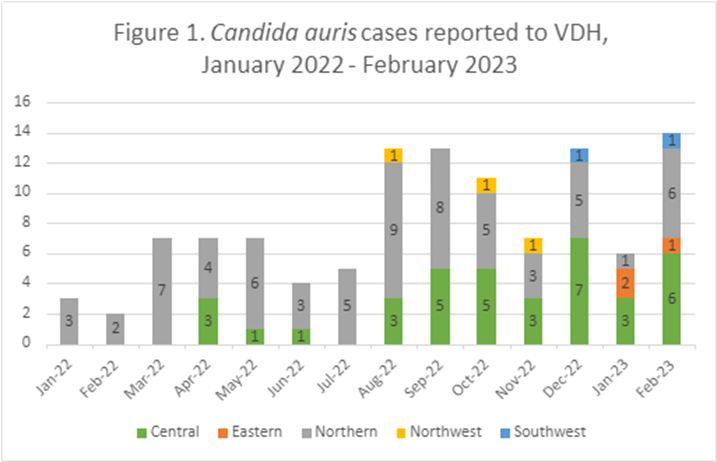
Source – Cases – Virginia Electronic Disease Surveillance System, data entered by 3/14/2023. Data is preliminary and subject to change.
CPOs and C. auris can cause asymptomatic colonization in patients, which can later lead to infection and transmission of the organism to other patients within a healthcare facility. Co-colonization of CPOs and C. auris has also been frequently observed. CPOs are highly antibiotic-resistant organisms that can cause infections that are difficult to treat, and in some cases, infections are resistant to all classes of available antibiotics.
Patients at highest risk for C. auris and/or CPO colonization are those who reside in or who have had prolonged admissions to high-risk healthcare facilities (particularly long-term acute care hospitals or ventilator-capable skilled nursing facilities). Persons who have recently spent time in hospitals and have invasive devices (e.g., mechanical ventilation or tracheostomy, feeding tubes, or central venous catheters) are also at high risk.
Prompt implementation of infection prevention and control measures is essential to prevent patient-to-patient transmission of C. auris and CPOs in healthcare settings. VDH recommends the following actions for health care providers:
- Be aware auris and CPO cases are on the rise and are causing outbreaks in healthcare facilities. Every region of the state has identified persons infected or colonized with C. auris or CPOs.
- Review and implement prevention measures to limit the spread of C. auris and CPOs as recommended on the CDC C. auris website and the CDC Carbapenem-resistant Enterobacterales website.
- Inquire about high-risk exposures in all newly admitted patients and consider auris and CPO screening and/or empiric contact precautions in patients at high risk, including those who:
- Had close contact in a healthcare setting to someone diagnosed with auris or CPO infection or colonization.
- Were admitted from a long-term acute care hospital or a ventilator-capable skilled nursing facility.
- Had international healthcare exposure within the past year.
- Immediately report any suspected or confirmed auris or CPO cases to public health by contacting your local health department per the Virginia Reportable Disease List.
- Ensure the implementation of appropriate infection prevention and control practices:
- All healthcare workers should have high adherence to hand hygiene.
- Patients with suspected or confirmed auris or CPOs in healthcare facilities should be managed using contact precautions. Some residents in nursing homes might be eligible to be managed with enhanced barrier precautions instead of contact precautions.
- When auris is suspected, use healthcare grade disinfectants that are registered with EPA for claims against C. auris (List P). Additionally, high-risk healthcare facilities should consider switching to a List P product prior to identification of C. auris due to increasing cases in Virginia.
- Use checklists to identify who is responsible for cleaning each item and cleaning frequency (e.g., environmental services staff versus clinical staff).
- Reinforce and audit core infection prevention practices in healthcare facilities.
- Conduct periodic education on multi-drug resistant organisms and training on appropriate infection prevention and control practices to healthcare workers.
- Communicate information about colonization or infection with auris or CPOs during care transitions within and transfers between healthcare settings.
Thank you for your partnership in HAI/AR prevention.
Sincerely,
Laurie Forlano, DO, MPH
Acting State Epidemiologist
Acting Director, Office of Epidemiology


